FIGHTING TO END INSURER ABUSE
We work at the intersection of policy, data, and real-world experience to challenge the insurer-driven system hollowing out American healthcare.

A Message from our Founder
When you’ve spent 20 years inside this system, you see exactly where it’s rigged.
 After more than two decades in the trenches of revenue cycle management, I’ve seen how insurance corporations, and the system built to serve them, have made it progressively harder to deliver and receive affordable, quality care.
After more than two decades in the trenches of revenue cycle management, I’ve seen how insurance corporations, and the system built to serve them, have made it progressively harder to deliver and receive affordable, quality care.
More and more costs are pushed onto patients. Medical debt is skyrocketing, leading many people to avoid even basic care. Providers are crushed under endless prior authorizations, delayed or denied payments, and relentless administrative burden. Hospitals and private practices close daily, unable to remain financially viable. And with insurance corporations making their lives increasingly difficult, more and more physicians are making the choice to leave the field on their own, exacerbating the shortage. Meanwhile, insurers grow richer, lobbyists write the rules, and legislation is continually shaped to protect insurance profits, not patients and providers.
Over time, it became clear to me that while empathetic patient collections, denial management, and claim-by-claim work remain essential, the problem goes far beyond administrative red tape. There’s a power imbalance baked into our healthcare laws, our payer contracts, and the system itself.
That’s why, in 2023, I decided to make advocacy a core part of what we do here. We still fight tooth and nail for every reimbursement. But I knew I needed to take the fight upstream.
With focused research and strategic advocacy, we bring to light the systemic barriers facing providers and patients, and work to advance policy solutions that protect care over insurance profit.
Yes, the odds are intentionally stacked in favor of insurance corporations. But we know how to push back, and we’re not letting up.
Our Current Focus
Our advocacy work is spearheaded by Write-Off Warrior, the in-house initiative we created to take on the system behind the billing. The name started as an internal moniker for our founder – but it stuck, and it’s become our banner for pushing back.
Here’s where our fight is focused right now:
Ending 20+ Years of Medicare Advantage Abuse
The Medicare Modernization Act of 2003 was supposed to expand access and promote innovation. Two decades later, we’ve drifted far from that promise. Instead of choice and competition, we have consolidation and corporate control. Instead of affordable care, we have higher costs, fewer options, and a system that favors insurers over patients and providers.
At the center of the problem is Medicare Advantage. These plans now cover over half of all Medicare beneficiaries, but they operate with fewer rules, less oversight, and far more denials than Traditional Medicare. Prior authorization abuse, delayed payments, billing manipulation, and rural exclusion have become the norm. The problem is especially pervasive for rural hospitals, as detailed in our piece for the Atlanta Journal-Constitution.
That’s why we’re pushing for a focused, commonsense fix: An oversight board for Medicare Advantage.
Traditional Medicare already operates under strict scrutiny.
Claims are reviewed, payments are audited, fraud is investigated, and taxpayer dollars are protected, all through a Medicare Administrative Contractor (MAC). Why shouldn’t Medicare Advantage be held to the exact same standards? We’re working hard to build legislative and citizen support for a similar oversight board – a Medicare Advantage MAC – to finally hold insurers accountable for these private plans.
Naturally, insurance lobbyists are already pushing back. After all, this threatens the billions they extract through unchecked denials, inflated risk scores, and delayed care, not to mention the billions of taxpayer dollars they steal each year through fraud and abuse, as uncovered by The Wall Street Journal.
But we’re not backing down. We’ve already met with the offices and policy teams of several Senators and Congresspeople who’ve committed to joining this fight. And we’ll keep the momentum going until Medicare Advantage insurers are finally held accountable.
Are you a provider struggling against Medicare Advantage abuses?
Share your story and get the tools to find a way out.

Our Latest Research
Working with our rural hospital clients, we hear the same concerns again and again – revenue held hostage by payers, essential staff stretched thin, and entire service lines disappearing just to keep the doors open.
We wanted to understand how widespread these issues really are, and whether any meaningful action was possible. So we expanded the conversation to a nationwide survey of rural hospital leaders, aiming to get the 30,000-foot insight into what’s happening on the ground, and why rural hospitals are closing at such alarming rates.
We invite you to see the findings for yourself, and to join the growing call for change.

Spreading the Word, Building the Movement
As we dug deeper into the extent of insurer abuse (and the lengths these corporations go to keep the odds so dramatically stacked in their favor) we understood that real and sustained change could only come from the power of millions of voices, not just a handful of us yelling into the void.
So Mark decided to take the show on the road, speaking at healthcare conferences, on podcasts, and at industry events around the country. Most of his presentations focus on a big-picture understanding of how we got into this mess, and how, with sustained effort and grassroots support, we can get out. He also spends plenty of time at each event sharing the pinpointed strategies providers can use right away to reduce administrative load and claw back rightfully owed reimbursements.
The more providers understand the backdoor mechanics of how the system really works – and the tools they can use to fight it – the better equipped they are to push back. The louder we get, and the more voices that join the fight, the sooner we’ll see real change.
Curious if Mark is a fit for your group? Click below for a quick exploratory call.
What Else We’re Working On
While our primary focus right now is Medicare Advantage reform, we’re also tracking other industry practices and policy trends that hurt patients and providers. As usual, the worst damage is being done quietly, in fine-print contracts, under layers of bureaucracy, and with little public awareness. That’s why we continue digging, listening, and exposing what needs to change.
Tracking the Latest Assault on Medicaid
Congressional leaders are once again proposing deep cuts to Medicaid as part of the budget reconciliation bill. These proposals include slashing federal funding, capping payments, and adding barriers to coverage that would push millions off the rolls. While our representatives continue to pretend this is about fiscal responsibility and efficiency, the real goal is to funnel yet more money to billionaires and massive corporations.
The proposed cuts would hit rural providers and safety net hospitals hardest, and the impact on patient access would be immediate. The focus is on looting the government coffers, not on true reform. We will continue to watch this closely, call out the greed, and fight for patients and providers.
For more details on this issue, please see Mark’s article, “Punish the Greed, Not Patients in Need.”
Addressing the Physician Exodus
Doctors are leaving the profession in record numbers, burned out and suffering the moral injury of a system that puts insurer profits ahead of patient care. We’re pushing for targeted reforms that put medicine back in the hands of physicians, not corporate middlemen. These include modernizing prior authorization rules, adjusting Medicare reimbursement to stop punishing independent providers, and supporting site-neutral payment policies that make it possible for physicians to practice with autonomy and integrity.
Learn more about the alarming physician shortage in Mark’s article, “It’s More Than Burnout. Doctors Are Ailing.”
Sounding the Alarm on Pharmacy Benefit Managers
Created by big insurance as a workaround to drug pricing regulation, PBMs now control which medications are covered, how much they cost, and how much pharmacies get paid. And of course, they operate with almost no transparency. One of their most damaging tactics is the use of Direct and Indirect Remuneration (DIR) fees, post-sale clawbacks that can wipe out any profit on a prescription. This is especially damaging for independent pharmacies, more of which are closing every day. We’re working with providers and policy allies to expose the impact of DIR fees, connect with lawmakers on the need for reform, and push for basic transparency standards that hold PBMs accountable.
Following the Money
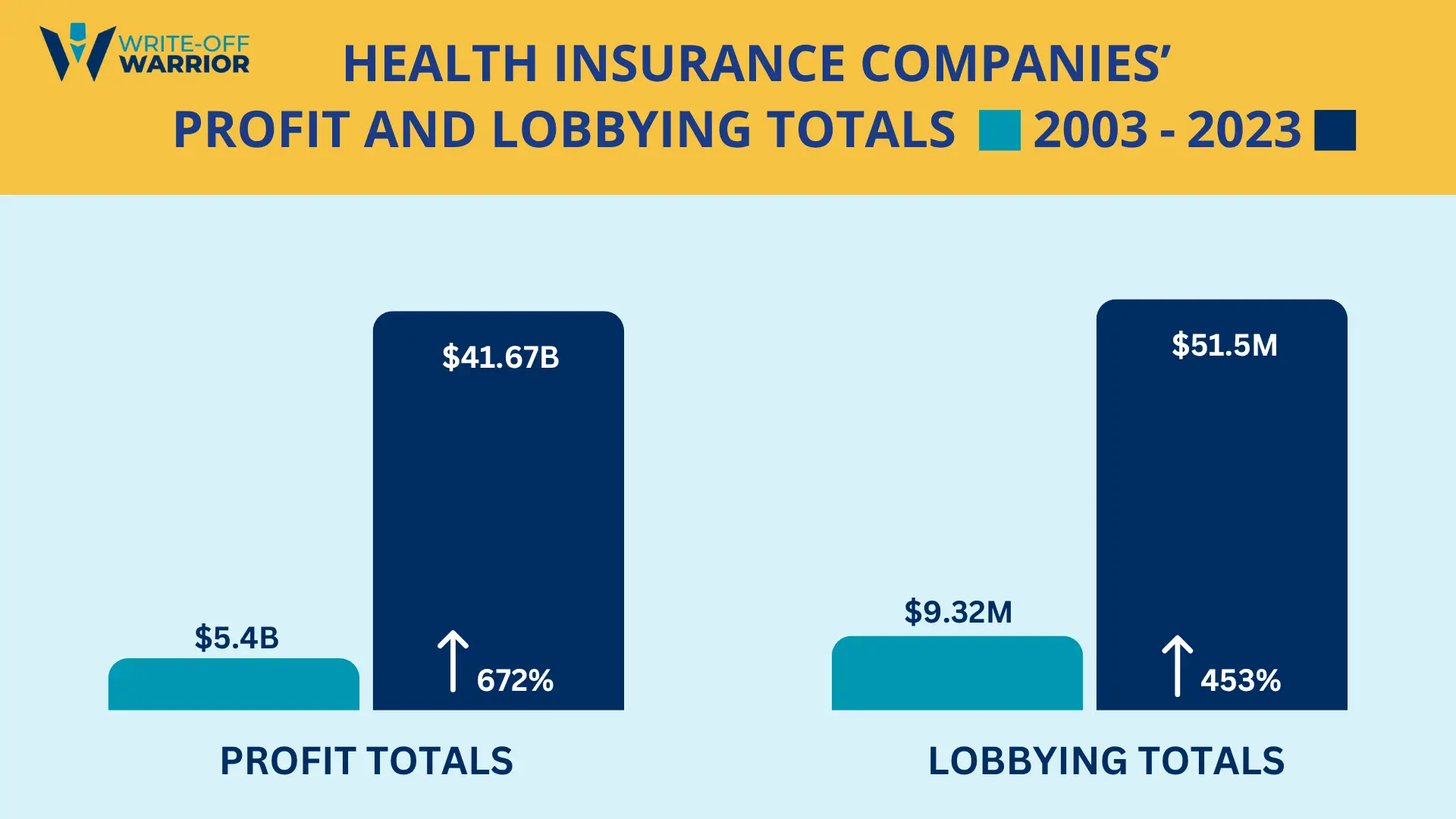
Everyone knows insurance corporations rake it in at provider and taxpayer expense. But the actual numbers are staggering. In 2023 alone, the six largest insurers pulled in over $40 billion in profit – a staggering 672% increase from 2003. And they spent more than $51 million lobbying Congress to keep the system working in their favor.
We think it’s important the public understands just how much these corporations benefit from delaying payments, dictating the terms of coverage, shoving more and more costs onto patients, preventing us from accessing lifesaving care, and pilfering taxpayer dollars that rightfully belong to Medicare and Medicaid. We’re tracking the money to keep the public informed and the pressure on.
What’s Next
Plans for future projects include state-by-state comparisons of denial rates, Medicaid Managed Care Organizations, and appeal outcomes; and deeper analysis of the financial fallout from ghost networks and out-of-network shifts.
How You Can Help
One quick, simple action you can take right now is to contact your representatives and let them know you support basic oversight for Medicare Advantage plans. Here’s a simple script you can modify as you like:
“I’m a voter in your district, and I’m furious after learning about the billions of taxpayer dollars fraudulently raked in by Medicare Advantage insurers. These companies are making money by inflating diagnoses and billing taxpayers for care people never even got. And then I found out they basically operate with no real oversight. They can deny care, underpay providers, and cook the books, while Traditional Medicare has strict rules and boards that review claims, investigate fraud, and make sure payments are fair. Why on earth don’t Medicare Advantage plans have to follow the same rules? Is there any reason you wouldn’t support holding them to the exact same standards?”
Your voice matters more than you think. Every call or email chips away at the silence these companies count on.
How You Can Help
One quick, simple action you can take right now is to contact your representatives and let them know you support basic oversight for Medicare Advantage plans. Here’s a simple script you can modify as you like:
“I’m a voter in your district, and I’m furious after learning about the billions of taxpayer dollars fraudulently raked in by Medicare Advantage insurers. These companies are making money by inflating diagnoses and billing taxpayers for care people never even got. And then I found out they basically operate with no real oversight. They can deny care, underpay providers, and cook the books, while Traditional Medicare has strict rules and boards that review claims, investigate fraud, and make sure payments are fair. Why on earth don’t Medicare Advantage plans have to follow the same rules? Is there any reason you wouldn’t support holding them to the exact same standards?”
Your voice matters more than you think. Every call or email chips away at the silence these companies count on.

Common-Sense Healthcare Reform Should Be Bi-Partisan
We’re working in a time of deep political dysfunction. Public trust in government is near historic lows. Misinformation spreads faster than facts. Congress remains in perpetual gridlock, even as the problems facing patients and providers grow ever more urgent. It may feel hopeless that any meaningful reform, especially the kind that challenges the interests of Big Insurance, can make it out of committee.
Nonetheless, we remain committed to urging legislators on both sides of the aisle to take basic and essential steps toward oversight, fairness, responsible stewardship, and bipartisanship, all long-held American values the public still hopes to see restored.
Are you a provider open to sharing your stories and challenges?
Together, we can connect the dots and drive change where it counts.